Why Your Gut Needs a Reset
Bloating after meals. Unpredictable bowel habits. That persistent feeling of sluggishness that no amount of coffee seems to fix. If these symptoms sound familiar, you’re not alone. Digestive complaints rank among the most common reasons people visit their primary care physicians, and the numbers continue climbing.
Modern life presents a perfect storm for gut disruption. Ultra‑processed foods now constitute over half of caloric intake in many Western diets. Chronic stress keeps the nervous system in overdrive, directly impairing digestive function. Sedentary work, erratic eating schedules, and insufficient sleep compound the problem further.
Here’s the encouraging reality: your gut possesses remarkable resilience. With the right approach, most people can significantly improve digestion naturally within weeks rather than months. A gut reset isn’t a crash detox or extreme cleanse promising miraculous overnight transformation. Instead, it represents a structured period of intentional dietary and lifestyle modifications designed to reduce irritation, support beneficial gut bacteria, and restore digestive rhythm. Think of it as pressing pause on habits that harm your gut while systematically introducing practices that heal it.
What a “Gut Reset” Really Is (and Isn’t)
The wellness industry has muddied the waters around gut health, promoting everything from juice fasts to expensive supplement protocols as essential “cleanses.” Let’s establish clarity: an evidence‑based gut reset focuses on removing dietary irritants, increasing fiber and plant diversity, supporting the microbiome with prebiotic and probiotic foods, and adopting lifestyle habits that enhance digestive function.
What it isn’t: a punishment, a starvation protocol, or a requirement to purchase specific branded products. Legitimate gut reset approaches align with recommendations from gastroenterologists and registered dietitians—whole foods, adequate fiber, proper hydration, stress management, and physical activity.
How Digestion and the Microbiome Work Together
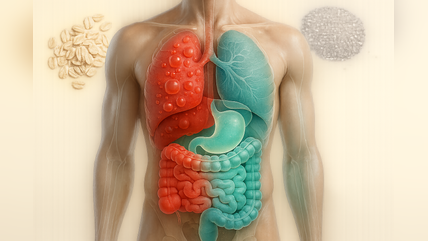
Understanding basic digestive mechanics helps explain why certain reset strategies work. Digestion begins in your mouth, where chewing and salivary enzymes start breaking down food. The stomach continues this process with acid and enzymes, transforming meals into a semi‑liquid mixture that moves into the small intestine. Here, most nutrient absorption occurs with help from pancreatic enzymes and bile.
The large intestine hosts the gut microbiome — trillions of bacteria, fungi, and other microorganisms that perform functions your body cannot accomplish alone. These microbes ferment dietary fiber into short‑chain fatty acids that nourish intestinal cells, synthesize certain vitamins, train the immune system, and even produce neurotransmitters affecting mood and cognition.
When this ecosystem falls out of balance — through poor diet, antibiotic use, chronic stress, or other factors — digestive symptoms often follow. A gut reset aims to restore conditions favoring beneficial microbes while reducing populations of potentially problematic organisms.
Doctor‑Approved Foundations for Better Digestion
Before diving into specific phases, understand the core pillars that virtually all digestive health experts agree upon. These foundations apply whether you’re doing a formal reset or simply want to improve digestion naturally over time.
Whole, Minimally Processed Foods as Your Base
Patterns rich in vegetables, fruits, whole grains, legumes, nuts, and seeds consistently associate with better digestive outcomes and greater microbiome diversity. These foods provide the raw materials your gut needs: fiber for microbial fermentation, polyphenols with anti‑inflammatory properties, and a range of vitamins and minerals supporting intestinal integrity.
Conversely, ultra‑processed foods — characterized by long ingredient lists featuring additives, emulsifiers, and artificial sweeteners — have been linked to reduced microbiome diversity and increased intestinal permeability. You don’t need to achieve perfection, but shifting the balance toward whole foods creates meaningful change.
Fiber – Your Gut’s Favorite Fuel
Fiber deserves special attention because most adults consume far less than recommended amounts. Current guidelines suggest 25 to 38 grams daily, yet average intake hovers around 15 grams.
Soluble fiber dissolves in water, forming a gel-like substance that slows digestion, helps regulate blood sugar, and feeds beneficial bacteria. Sources include oats, barley, beans, lentils, apples, and citrus fruits. Insoluble fiber adds bulk to stool and accelerates transit through the colon. Whole wheat, nuts, vegetables, and the skins of many fruits provide insoluble fiber.
The key principle: increase fiber gradually. Adding too much too quickly overwhelms the system and causes the very gas and bloating you’re trying to resolve. Aim to add roughly 3–5 grams per week until reaching your target.
Hydration and Digestive Motility
Water plays an under‑appreciated role in digestive health. Adequate hydration keeps stool soft and supports regular transit time. Fiber without sufficient water can actually worsen constipation rather than relieve it.
While individual needs vary based on activity level, climate, and body size, most adults benefit from consuming approximately eight 8‑ounce glasses daily as a baseline. Increase this amount when adding fiber supplements or during hot weather.
The Gut Reset Blueprint – 7 to 21‑Day Step‑by‑Step Plan
This gut reset plan spans anywhere from one to three weeks depending on your starting point, symptoms, and goals. Those with mild digestive complaints may notice improvement within the first week. Others with more entrenched issues benefit from the full 21‑day protocol.
Important caveat: if you have diagnosed conditions like inflammatory bowel disease, celiac disease, or other serious medical issues, consult your healthcare provider before making significant dietary changes.
Phase 1 – Gentle Clean‑Up (Days 1–3)
The initial phase focuses on removing or sharply reducing substances that commonly irritate the digestive tract. This isn’t about deprivation — it’s about giving your gut breathing room.
During these three days, eliminate or minimize ultra‑processed foods, sugary beverages, excess alcohol, and any foods you suspect trigger your symptoms. Focus on simple, easy-to-digest meals: cooked vegetables, lean proteins, rice, eggs, and small amounts of ripe fruit.
Keep meals moderate in size and well‑spaced throughout the day. Avoid eating within two to three hours of bedtime. Stay well‑hydrated, but limit fluids during meals to avoid diluting digestive secretions.
Phase 2 – Rebuild and Nourish (Days 4–14)
With the initial clean‑up complete, phase two gradually reintroduces more diverse plant foods while layering in specific gut‑supporting elements.
Begin adding more fiber‑rich vegetables, fruits, and whole grains—always incrementally. Introduce prebiotic foods like onions, garlic, leeks, asparagus, and slightly green bananas that feed beneficial bacteria. If tolerated, include fermented foods such as plain yogurt with live cultures, kefir, sauerkraut, or kimchi.
This phase also emphasizes routine. Eating meals at consistent times helps regulate digestive rhythms. Prioritizing seven to eight hours of sleep supports the gut‑brain axis and overnight repair processes. Continue avoiding known trigger foods and excessive alcohol.
Phase 3 – Personalize and Maintain (Days 15–21 and Beyond)
The final phase transforms your reset into a sustainable long‑term approach. By now, you’ve identified foods and habits that support your digestion.
Systematically reintroduce any foods you eliminated during phase one, one at a time, with several days between introductions. This methodical approach helps identify specific triggers rather than guessing. Keep a simple food and symptom journal to track patterns.
Create your personalized maintenance plan incorporating the foods, meal timing, and lifestyle practices that worked best during the reset. This isn’t a temporary diet — it’s a template for ongoing digestive wellness.
Doctor‑Approved Food Strategies for Better Digestion
Beyond the general framework, specific food strategies offer targeted digestive benefits.
Prebiotic‑Rich Foods to Feed Your Good Bacteria
Prebiotics are non‑digestible food components that selectively stimulate growth of beneficial gut bacteria. Top sources include Jerusalem artichokes, chicory root, dandelion greens, garlic, onions, leeks, asparagus, bananas (especially slightly unripe), oats, apples, and legumes.
Aim to include at least one prebiotic‑rich food at most meals. Cooking may reduce some prebiotic content, so incorporate raw options when tolerable.
Probiotic Foods and Fermented Staples
While prebiotic foods feed existing beneficial bacteria, probiotic foods introduce live microorganisms directly. Yogurt with live active cultures, kefir, traditionally fermented sauerkraut and kimchi, miso, tempeh, and kombucha all qualify.
Include fermented foods regularly — daily if well‑tolerated. Start with small portions if you’re new to fermented foods, as some people initially experience increased gas. Those with histamine intolerance or small intestinal bacterial overgrowth may need to limit fermented foods and should work with a healthcare provider.
Fats, Proteins, and Carbs – Balancing Your Plate for Easier Digestion
Balanced meals digest more smoothly than those heavily skewed toward any single macronutrient. Include healthy fats from olive oil, avocado, nuts, and fatty fish to support satiety and nutrient absorption. Choose lean proteins that won’t overtax digestive capacity. Pair complex carbohydrates with protein and fat to slow gastric emptying and prevent blood sugar spikes.
A practical template: fill half your plate with vegetables, one quarter with protein, and one quarter with whole grains or starchy vegetables, adding a modest amount of healthy fat.
Lifestyle Habits That Reset and Support Your Gut
Food matters enormously, but non‑dietary factors significantly influence digestive function.
Eating Hygiene – How You Eat Matters
Slowing down and chewing thoroughly are simple interventions with profound effects. Thorough chewing mechanically breaks down food and mixes it with salivary enzymes, reducing the burden on your stomach and intestines.
Practice mindful eating by putting utensils down between bites, avoiding screens during meals, and paying attention to hunger and fullness cues. Avoid large meals close to bedtime, which can promote reflux and disrupt sleep quality.
Daily Movement and Post‑Meal Activity
Physical activity stimulates intestinal motility and helps move gas through the digestive tract. Even a ten‑ to fifteen‑minute walk after meals can significantly reduce bloating and support healthy transit.
Regular exercise—whether walking, swimming, cycling, or strength training—benefits gut health beyond immediate meal‑related effects. Movement reduces stress hormones, improves sleep, and may positively influence microbiome composition.
Stress, Sleep, and the Gut‑Brain Axis
The gut and brain communicate bidirectionally through what researchers call the gut‑brain axis. Chronic stress activates the sympathetic nervous system, shunting resources away from digestion and slowing motility. Poor sleep disrupts circadian rhythms that govern digestive processes and alters the microbiome.
Stress management strategies like deep breathing, meditation, yoga, time in nature, and adequate leisure time directly benefit digestive function. Prioritize consistent sleep schedules and good sleep hygiene practices.
Smart Use of Supplements in a Gut Reset (Optional, Not Required)
Supplements can serve as helpful tools but should never substitute for dietary and lifestyle foundations. Consider them optional additions rather than requirements.
Fiber Supplements (Psyllium, Partially Hydrolyzed Guar, etc.)
Fiber supplements help those struggling to meet intake goals through food alone. Psyllium husk, a soluble fiber, has strong evidence for improving regularity and may benefit cholesterol levels. Partially hydrolyzed guar gum causes less bloating for some individuals.
Introduce any fiber supplement slowly, take with plenty of water, and separate from medications by at least two hours to avoid absorption interference.
👉 For a simpler, doctor‑formulated option: [Gut Optim – a fiber & microbiome support formula]
Probiotics and Synbiotics
Probiotic supplements may help specific situations: restoring balance after antibiotic courses, managing certain IBS symptoms, or supporting immunity. However, strain specificity matters — different bacterial strains produce different effects.
Synbiotics combine probiotics with prebiotics to potentially enhance survival and colonization of beneficial organisms. Look for products with clinically studied strains and adequate colony‑forming units.
💡 Prefer a professionally formulated option rather than random pills? Consider [Gut Optim’s synbiotic blend] for balanced microbiome support.
When a DIY Gut Reset Isn’t Enough – Red Flags and Doctor Visits
Self‑directed gut resets work well for general digestive optimization, but certain symptoms require professional evaluation.
Red‑Flag Symptoms You Shouldn’t Ignore
Seek medical attention for unexplained weight loss, blood in stool, severe or persistent abdominal pain, frequent vomiting, difficulty swallowing, signs of anemia, or symptoms that wake you from sleep. These may indicate conditions requiring diagnosis and treatment beyond lifestyle modification.
Getting Proper Testing and Diagnosis
Gastroenterologists and primary care physicians can perform appropriate evaluations including detailed history, physical examination, laboratory tests, breath tests for bacterial overgrowth or carbohydrate malabsorption, imaging studies, and endoscopic procedures when indicated. Accurate diagnosis should precede any restrictive dietary approach.
Frequently Asked Questions – Gut Reset Blueprint
How long does a gut reset take to notice results? Many people experience improvements in bloating and regularity within the first week. More substantial changes to microbiome composition and overall digestive function typically require three to four weeks of consistent effort.
Can I improve my digestion naturally without cutting out entire food groups? Absolutely. Most evidence‑based approaches emphasize addition — more fiber, more plant diversity, more fermented foods — rather than elimination. Only remove specific foods if you’ve identified them as personal triggers.
Is a gut reset safe if I have IBS, IBD, or reflux? Modified approaches can be safe and beneficial, but work with your healthcare team. Those with IBD should be particularly cautious about fiber increases during flares.
Do I need probiotics to reset my gut? No. Probiotic‑rich foods and prebiotic fiber support microbiome health effectively for most people. Supplements remain optional.
Can a gut reset help with bloating and gas? Yes, particularly when combined with slower eating, gradual fiber increases, and identification of personal trigger foods.
How often should I do a gut reset? Rather than repeated resets, aim to incorporate the principles into your regular lifestyle. Some people find a brief reset helpful seasonally or after periods of dietary indiscretion.
Putting It All Together – Your Personalized Gut Reset Blueprint
Improving digestion naturally doesn’t require complicated protocols or expensive interventions. The formula is straightforward: clean up your diet by reducing processed foods and irritants, rebuild digestive capacity with diverse fiber-rich plants and fermented foods, then personalize your approach based on what your body tells you.
Keep a simple symptom journal throughout your reset. Notice what helps. Notice what doesn’t. Adjust your pace—moving faster if you’re responding well, slowing down if symptoms flare. Seek professional guidance when needed, especially if red‑flag symptoms appear.
Your gut reset blueprint is ultimately yours to customize. The strategies outlined here provide the evidence‑based framework; your personal experimentation refines it into a sustainable plan that supports your digestive health for years to come.
Want help getting started?
I created Gut Optim — a targeted fiber and microbiome support formula — to make this process easier.
Read The Full Gut Optim Review →https://healthdigest.blog/gutoptimreview/