Why Bloating and Gas Are So Common
If you’re reading this while feeling uncomfortably bloated, you’re far from alone. Studies suggest that up to 30% of adults experience regular bloating, with some surveys showing even higher rates among those with digestive conditions. This uncomfortable sensation of abdominal fullness, tightness, or visible distension affects millions daily, significantly impacting quality of life, social activities, and overall wellbeing.
The frustration many people feel stems from bloating’s unpredictable nature and the confusion surrounding its causes. One day you feel fine; the next, you look six months pregnant after eating seemingly innocent foods. This guide will help you understand what’s actually happening in your digestive system, provide immediate relief strategies you can use today, and outline evidence-based long-term solutions for managing bloating and gas effectively.
Understanding Bloating and Gas – What’s Actually Happening in Your Gut
Before diving into solutions, it’s crucial to understand the mechanics behind bloating and gas. Your digestive system naturally produces gas as bacteria in your gut break down food. This process typically generates between 0.5 to 1.5 liters of gas daily, most of which gets absorbed into the bloodstream or expelled without you noticing.
Bloating occurs when this delicate balance gets disrupted. The sensation involves two components: subjective bloating (feeling full or tight) and objective abdominal distension (measurable increase in abdominal girth). Interestingly, these don’t always occur together – you can feel bloated without visible swelling, or have distension without discomfort.
Gas accumulates in your digestive tract through three main routes: swallowing air while eating or drinking, bacterial fermentation of undigested food in your colon, and diffusion of gas from your bloodstream into your intestines. When gas movement slows or production increases, you experience the characteristic pressure, pain, and visible swelling of bloating.
Typical Causes of Everyday Bloating and Gas
The most common culprit behind functional bloating is irritable bowel syndrome (IBS), affecting 10-15% of the global population. IBS causes heightened gut sensitivity and altered motility, leading to gas retention and painful bloating even with normal gas volumes. Women with IBS often report worse symptoms around menstruation due to hormonal influences on gut function.
Food intolerances rank second among bloating triggers. Lactose intolerance affects approximately 68% of the world’s population to varying degrees, causing gas, bloating, and diarrhea when dairy products aren’t properly digested. FODMAPs (fermentable oligosaccharides, disaccharides, monosaccharides, and polyols) represent another category of poorly absorbed carbohydrates that ferment rapidly in the gut, producing excess gas. Common high-FODMAP foods include wheat, onions, garlic, beans, and certain fruits.
Constipation creates a vicious cycle with bloating. When stool moves slowly through your colon, bacteria have more time to ferment its contents, producing extra gas. The backed-up stool also physically contributes to distension and discomfort. Even mild constipation can significantly worsen bloating symptoms.
Aerophagia, or excessive air swallowing, contributes more to bloating than many realize. Eating quickly, drinking through straws, chewing gum, smoking, and wearing loose dentures all increase air intake. Anxiety and stress can also trigger unconscious air swallowing, explaining why bloating often worsens during stressful periods.
When Bloating May Signal a Medical Condition
While most bloating is benign, certain patterns warrant medical evaluation. Celiac disease, affecting about 1% of the population, causes severe bloating along with diarrhea, weight loss, and nutritional deficiencies when gluten triggers intestinal inflammation. Unlike temporary bloating from food intolerances, celiac-related symptoms progressively worsen without strict gluten avoidance.
Inflammatory bowel diseases like Crohn’s disease and ulcerative colitis cause chronic inflammation that disrupts normal digestion and gas processing. These conditions typically present with bloody stools, persistent diarrhea, unexplained weight loss, and fever alongside bloating.
More serious but less common causes include intestinal obstruction (causing severe pain and vomiting), ovarian tumors (particularly concerning in postmenopausal women with new-onset bloating), liver disease (accompanied by jaundice or ascites), and pancreatic disorders affecting enzyme production. These conditions require prompt medical attention and shouldn’t be self-diagnosed.
Quick Relief: What Helps Bloating and Gas Fast
When bloating strikes, you need relief now, not next week. These evidence-based strategies can provide comfort within minutes to hours.
Positioning, Movement and Gentle Exercises
Physical movement remains one of the fastest, most effective ways to relieve gas and bloating. Walking for just 10-15 minutes after meals helps stimulate intestinal contractions, moving trapped gas through your system. This simple intervention shows consistent benefits across multiple studies.
The knee-to-chest position specifically targets gas relief by gently compressing your abdomen and encouraging gas movement. Lie on your back, bring one knee toward your chest, hold for 20 seconds, then switch legs. Repeat this cycle 5-10 times, finishing by hugging both knees simultaneously.
Certain yoga poses excel at relieving gas. Child’s pose gently massages abdominal organs while promoting relaxation. Cat-cow stretches mobilize your spine and massage internal organs. Twisted poses like supine spinal twist help “wring out” trapped gas. Practice these poses gently, breathing deeply throughout.
Diaphragmatic breathing offers dual benefits: reducing stress-related bloating and physically massaging your intestines. Place one hand on your chest, another on your belly. Breathe slowly through your nose, expanding your belly rather than your chest. Exhale slowly through pursed lips. Practice for 5-10 minutes when bloating occurs.
Over-the-Counter Options and Home Remedies
Simethicone, found in products like Gas-X, works by breaking up gas bubbles in your digestive tract, making them easier to expel. While studies show mixed results for bloating relief, many people find it helpful for gas-related discomfort. Follow package directions carefully.
Peppermint oil demonstrates more robust evidence for IBS-related bloating. Its antispasmodic properties relax intestinal muscles, easing gas passage and reducing pain. Choose enteric-coated capsules to prevent heartburn, and avoid peppermint if you have GERD, as it can worsen reflux symptoms.
Activated charcoal theoretically absorbs excess gas, though scientific evidence remains limited. If trying it, take it away from medications and supplements, as it can interfere with absorption. Start with small doses to assess tolerance.
Traditional herbal teas offer gentle relief for many people. Ginger tea reduces nausea and may speed gastric emptying. Fennel and chamomile teas have carminative properties, helping expel gas. Drink these warm, not hot, sipping slowly to avoid swallowing extra air.
Simple Food and Drink Tweaks for Same-Day Relief
Eliminating carbonated beverages provides immediate improvement for many bloating sufferers. The carbon dioxide in sodas, sparkling water, and beer directly contributes to gas accumulation. Replace these with still water or herbal teas for quick relief.
High-fat meals slow gastric emptying, prolonging fullness and bloating. For immediate relief, switch to lighter, lower-fat options. Choose grilled chicken over fried, skip creamy sauces, and limit cheese and butter. You’ll notice reduced bloating within hours.
Large meals stretch your stomach and overwhelm your digestive capacity. Instead of three large meals, try five or six smaller portions spread throughout the day. This reduces the digestive burden while maintaining steady energy levels.
Alcohol disrupts normal digestion and can trigger inflammation in sensitive individuals. Limiting or avoiding alcohol for a few days often dramatically improves bloating. When you do drink, alternate alcoholic beverages with water to minimize effects.
Diet Changes for Long-Term Bloating and Gas Control
While quick fixes provide temporary relief, lasting improvement requires addressing dietary triggers systematically.
The Role of FODMAPs and Food Intolerances
The low-FODMAP diet, developed at Monash University, helps identify specific fermentable carbohydrates triggering your symptoms. This three-phase approach starts with strict FODMAP elimination for 2-6 weeks, followed by systematic reintroduction to identify personal triggers, then long-term personalization.
Common high-FODMAP foods causing bloating include wheat products, dairy, onions, garlic, legumes, stone fruits, and artificial sweeteners. However, FODMAP sensitivity varies greatly between individuals. What devastates one person’s digestion might not affect yours at all.
Working with a registered dietitian trained in the low-FODMAP approach significantly improves success rates. They’ll ensure nutritional adequacy during elimination and guide proper reintroduction. Self-directed FODMAP restriction risks unnecessary dietary limitations and potential nutrient deficiencies.
Beyond FODMAPs, other food intolerances contribute to bloating. Gluten sensitivity (distinct from celiac disease), histamine intolerance, and specific food chemicals like salicylates can trigger symptoms. Keeping a detailed food and symptom diary helps identify patterns.
Fiber – How Much Is Too Little or Too Much?
Fiber plays a paradoxical role in bloating. Too little fiber causes constipation and subsequent bloating, while rapidly increasing fiber intake overwhelms your gut bacteria, causing excessive fermentation and gas.
Soluble fiber, found in oats, beans, and fruits, forms a gel-like substance that can initially increase bloating but ultimately improves bowel regularity and reduces symptoms long-term. Insoluble fiber from whole grains and vegetables adds bulk to stool but may worsen bloating in sensitive individuals.
The key lies in gradual adjustment. Increase fiber intake by 5 grams weekly, not daily. Spread fiber throughout the day rather than consuming large amounts at once. Most importantly, increase water intake proportionally – fiber without adequate hydration worsens constipation and bloating.
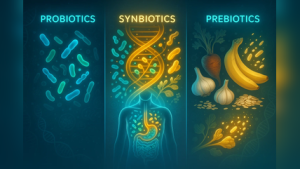
Probiotics, Prebiotics and Fermented Foods
Probiotics show promise for bloating relief, though effects vary by strain and individual. Bifidobacterium infantis and Lactobacillus plantarum demonstrate the strongest evidence for IBS-related bloating. Multi-strain formulations often work better than single strains.
Fermented foods like yogurt, kefir, sauerkraut, and kimchi provide natural probiotics along with beneficial postbiotics. Start with small servings, as some people initially experience increased gas before improvement. Choose varieties without added sugars, which can worsen bloating.
Prebiotics feed beneficial bacteria but can paradoxically worsen bloating initially. Foods high in prebiotics include garlic, onions, asparagus, and bananas – many of which are also high-FODMAP. If you’re sensitive, consider supplemental prebiotics like partially hydrolyzed guar gum, which causes less gas than traditional prebiotic foods.
Lifestyle Habits that Reduce Bloating and Gas
Beyond diet, daily habits significantly impact digestive comfort.
Eating Habits and Meal Patterns
Eating slowly might sound simplistic, but it’s remarkably effective. Taking 20-30 minutes per meal reduces air swallowing, improves digestion, and enhances satiety signals. Put your fork down between bites, chew thoroughly, and avoid eating while distracted by screens.
Meal timing matters more than most realize. Eating large dinners late in the evening doesn’t allow adequate digestion before lying down. Aim to finish eating 3-4 hours before bedtime. If you must eat late, keep portions small and easily digestible.
Avoid talking while chewing, as this increases air intake. Similarly, drinking through straws, chewing gum, and sucking on hard candies all contribute to aerophagia. Even seemingly harmless habits like pen-chewing or nail-biting increase swallowed air.
Physical Activity and Core/Diaphragmatic Work
Regular moderate exercise improves gut motility, reduces stress, and helps maintain healthy gut bacteria. Aim for 150 minutes of moderate activity weekly, but even 10-minute walks after meals provide benefits.
Core strengthening supports proper abdominal function and may reduce bloating. Planks, bridges, and gentle Pilates exercises strengthen without the high-intensity movements that can worsen symptoms during flares.
Diaphragmatic breathing exercises train your body’s relaxation response while physically supporting digestion. Practice twice daily when symptom-free to build the habit, making it easier to implement during bloating episodes.
Stress, Sleep and the Gut-Brain Axis
The gut-brain axis explains why stress and anxiety directly impact digestion. Stress hormones alter gut motility, increase intestinal permeability, and change bacterial composition – all contributing to bloating and gas.
Cognitive-behavioral therapy (CBT) specifically adapted for IBS shows remarkable success in reducing bloating. This therapy helps identify thought patterns and behaviors perpetuating symptoms, teaching practical coping strategies.
Poor sleep disrupts hormones regulating hunger and digestion, often worsening bloating. Prioritize 7-9 hours nightly, maintaining consistent sleep-wake times. Address sleep disorders like apnea, which can increase air swallowing and morning bloating.
When You Should See a Doctor About Bloating and Gas
While most bloating responds to self-care, certain situations require professional evaluation.
Red-Flag Symptoms You Shouldn’t Ignore
Unexplained weight loss accompanying bloating always warrants investigation. Losing more than 5% of body weight without trying could indicate inflammatory conditions, malabsorption, or malignancy.
Blood in stool, whether bright red or dark/tarry, requires immediate evaluation. While often from benign causes like hemorrhoids, it can signal serious conditions requiring prompt treatment.
Persistent vomiting with bloating suggests obstruction or severe gastroparesis. Fever indicates infection or inflammation. Severe, worsening abdominal pain differs from typical gas discomfort and shouldn’t be dismissed.
New-onset bloating in people over 50, especially women, deserves careful evaluation. Family history of gastrointestinal or gynecological cancers lowers the threshold for investigation.
What to Expect at a Medical Evaluation
Your doctor will take a detailed history, asking about symptom timing, triggers, and associated features. They’ll perform a physical examination, checking for tenderness, masses, or signs of obstruction.
Initial tests might include blood work checking for celiac antibodies, inflammatory markers, and thyroid function. Stool tests can identify infections, inflammation, or malabsorption. Breath tests diagnose lactose intolerance or small intestinal bacterial overgrowth.
If initial tests are inconclusive, imaging like ultrasound or CT scan may visualize structural abnormalities. Endoscopy allows direct visualization and biopsy of digestive tract tissues when inflammatory or malignant conditions are suspected.
Treatment Options Your Clinician Might Recommend
Medical management depends on underlying causes but often includes targeted approaches for functional bloating.
Targeted Medications and Therapies
For IBS-related bloating, antispasmodics like dicyclomine or hyoscyamine reduce cramping and may improve gas transit. Rifaximin, a non-absorbed antibiotic, shows particular promise for bloating in IBS, likely by modulating gut bacteria.
Secretagogues like lubiprostone or linaclotide help constipation-predominant IBS with bloating by increasing intestinal fluid secretion. Neuromodulators, including certain antidepressants at low doses, can reduce visceral hypersensitivity.
Gut-directed hypnotherapy achieves remarkable results for some patients, with benefits lasting years after treatment. This specialized therapy differs from general hypnosis, specifically targeting gut-brain communication.
Working with a Dietitian or Specialist
Registered dietitians specializing in digestive health provide invaluable support for complex cases. They ensure nutritional adequacy while eliminating triggers, preventing the common pitfall of overly restrictive diets.
Gastroenterologists offer specialized testing and treatments unavailable in primary care. Don’t hesitate to request referral if symptoms significantly impact your quality of life or don’t respond to initial management.
Frequently Asked Questions (FAQ) – Bloating and Gas Relief
What is the fastest way to relieve bloating and gas? Walking for 10-15 minutes provides the quickest natural relief. Combine this with the knee-to-chest position and gentle twisting stretches. Over-the-counter simethicone may help with gas, while peppermint oil capsules can ease IBS-related bloating.
Why do I get bloated every time I eat? Consistent post-meal bloating suggests food intolerances, rapid eating, or IBS. Keep a detailed food diary noting symptoms, timing, and severity. Consider working with a dietitian to identify triggers through systematic elimination and reintroduction.
How do I know if my bloating is serious? Seek medical attention for bloating with unexplained weight loss, blood in stool, persistent vomiting, severe pain, or fever. New-onset bloating after age 50 or family history of GI cancers also warrants evaluation.
Do probiotics actually help with gas and bloating? Certain probiotic strains show evidence for reducing IBS-related bloating, particularly Bifidobacterium infantis. However, effects vary between individuals. Try a multi-strain formula for 4-8 weeks to assess benefits.
What foods cause the most gas and bloating? Common triggers include beans, cruciferous vegetables, dairy products, wheat, onions, garlic, and artificial sweeteners. However, individual responses vary greatly. Your triggers might differ from typical patterns.
How long should I try diet changes before seeing a doctor? Give dietary modifications 4-6 weeks for full effect. However, see a doctor sooner if you experience red-flag symptoms or if bloating severely impacts your daily life.
Can stress alone cause bloating and gas? Absolutely. Stress directly affects gut motility, bacterial balance, and visceral sensitivity through the gut-brain axis. Many people experience complete resolution with stress management alone.
Is long-term bloating always a sign of IBS? While IBS is the most common cause of chronic bloating, other conditions like small intestinal bacterial overgrowth, gastroparesis, or food intolerances can cause similar symptoms. Proper evaluation helps determine the specific cause.
Putting It All Together: Your Personal Bloating and Gas Relief Plan
Creating an effective, personalized strategy for managing bloating requires a systematic approach. Start with immediate relief techniques when symptoms occur: walk for 10-15 minutes, practice diaphragmatic breathing, and try gentle yoga poses.
Simultaneously, begin a 2-4 week lifestyle modification trial. Eat slowly and mindfully, reduce portion sizes, avoid carbonated beverages, and limit high-fat foods. Incorporate regular physical activity and stress management techniques.
Track your symptoms meticulously using a diary or app, noting foods, stress levels, sleep quality, and symptom severity. Look for patterns emerging over time rather than focusing on day-to-day variations.
If symptoms don’t improve after a month of consistent lifestyle changes, or if you identify specific food triggers you can’t navigate alone, seek professional help. A registered dietitian can guide elimination diets safely, while a gastroenterologist can rule out underlying conditions.
Remember that managing bloating often requires patience and experimentation. What works for others might not work for you. Focus on evidence-based strategies while remaining attentive to your body’s unique responses. With the right combination of dietary modifications, lifestyle changes, and medical support when needed, most people achieve significant improvement in their bloating and gas symptoms.